NSAIDs for arthritis pain linked to increased risk of heart valve disease
11/25/2019 / By Edsel Cook
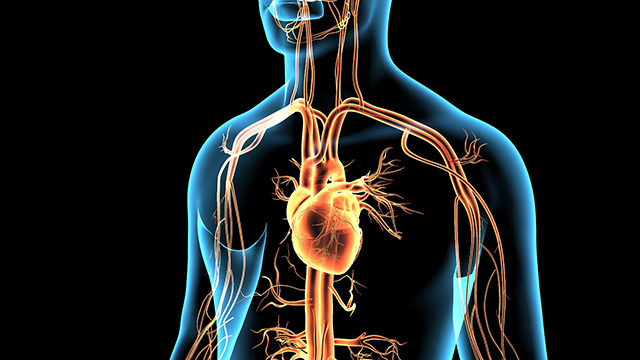
Arthritis patients often use celecoxib, a nonsteroidal anti-inflammatory drug (NSAID) for alleviating swelling and pain. But researchers warned that it might trigger serious issues in the aortic valve. Celecoxib goes by the brand name of Celebrex. It belongs to a group of NSAIDs called COX-2 inhibitors.
The Vanderbilt University research team evaluated multiple medical records. They found a link between celecoxib usage and the risk of developing aortic stenosis. Aortic stenosis is a condition where the aortic valve becomes narrower and stiffer. It often stems from damage to the blood vessel or calcification associated with aging.
The researchers also tested the effects of celecoxib on aortic valve cells. They found that the NSAID aggravated the calcification process. Their results conflicted with those of a 2016 study published in the New England Journal of Medicine (NEJM). The earlier report asserted that celecoxib was no more dangerous to the heart than the older NSAIDs ibuprofen and naproxen. The Vanderbilt team argued that the 2016 study concentrated on acute, short-term, and blood clot-related events. It didn’t consider valve disease, which develops over longer periods than thrombosis.
“In this study, we’re adding a long-term perspective on celecoxib use,” commented Vanderbilt researcher Dr. Meghan A. Bowler, the first author of the paper. (Related: Pilot study finds that resveratrol can be used as a complementary treatment with meloxicam for knee osteoarthritis.)
The NSAID celecoxib is not as safe for the heart as earlier studies assumed
The aortic valve joins the aorta and the left ventricle of the heart. Aortic stenosis stiffens this valve and makes it narrower. The cramped blood vessel makes it more difficult for the heart to pump blood into the aorta and the rest of the body. Some patients develop aortic stenosis due to a health issue at birth. But in most cases, the heart condition came from the accumulation of calcium deposits and scarred tissue in the aortic valve as a person got older.
In their paper, the Vanderbilt researchers found signs of calcification-induced aortic stenosis in more than one out of every four Americans older than 65 years. Aortic stenosis counted as a progressive disease. There were no pharmaceutical drugs that would reverse the effects of heart valve disease. The only conventional treatment involved a complicated surgical operation that replaced the aortic valve. Ironically, the lack of non-surgical treatments for aortic stenosis got Bowler’s team to investigate celecoxib – but as a possible therapeutic approach. Earlier studies indicated that the NSAID might be able to regulate cadherin-11, a protein involved in the disease.
Celebrex increases the risk of heart valve disease by 20 percent
The Vanderbilt researchers administered celecoxib to aortic valves taken from pigs. To their surprise, celecoxib didn’t reduce the markers of tissue stiffening associated with calcification. On the contrary, the pharmaceutical drug increased the number of calcium nodules and activated more myofibroblasts. These processes increased the stiffness of aortic valve tissue, thereby indicating that the NSAID aggravated aortic stenosis.
Bowler and her colleagues sought out clinical evidence that might support the results of their laboratory test. They pored over 8,600 long-term medical records for any connection between celecoxib, ibuprofen, and naproxen-based treatment and the confirmation of heart valve disease. They reported that celecoxib-based treatment led to a 20 percent increase in the risk of aortic stenosis. While ibuprofen and naproxen also harm the heart, the two older NSAIDs did not appear to be linked to heart valve disease.
“Overall, these data suggest that celecoxib use is associated with the development of [calcific aortic valve disease],” Bowler reported.
Sources include:
Submit a correction >>
Tagged Under:
anti-inflammatory, arthritis, heart health, heart valve disease, Non-steroidal anti-inflammatory drugs, NSAIDs, pain relief, Prescription drugs, research
This article may contain statements that reflect the opinion of the author
RECENT NEWS & ARTICLES
HeartDisease.News is a fact-based public education website published by Heart Disease News Features, LLC.
All content copyright © 2018 by Heart Disease News Features, LLC.
Contact Us with Tips or Corrections
All trademarks, registered trademarks and servicemarks mentioned on this site are the property of their respective owners.